by Editor | May 25, 2021 | Opinions
 By Mayur Abhaya Srisrimal,
By Mayur Abhaya Srisrimal,
Chennai : Most of the time parents are faced with myriad decisions for their newborns. One of them is whether to preserve their baby’s umbilical cord stem cells. It’s a decision most parents-to-be consider, weighing the cost against the potential future benefits which might help treat certain genetic diseases and cancers that your child may get.
The first successful umbilical cord blood stem cell transplant was done 28 years ago in France, and over the last 20 years more than 40,000 patients worldwide have had umbilical cord blood transplants. In India, there is increasing awareness about cases that are successfully treated with stem cells and this has led to umbilical cord banking to be a propagated as opposed to being discarded as medical waste.
Families wanting to improve their access to stem cells resort to preserving their baby’s umbilical cord blood stem cells at private stem cell banks, even though it provides only a 25 per cent chance of being a match for the siblings. Every year, approximately 100,000 units are preserved in such private banks.
Due to lack of financial support for public banking only approximately 5,000 cord blood units are available in public banks (<1 per cent of the global inventory for 20 per cent of the world’s population) which provides a very minimal chance of obtaining a suitable match.
Every year nearly 25,000 patients in India are unable to find a matching stem cell during times of need due to the low Indian inventory. Patients struggle to find a matching cord blood unit after trying their luck with other sources of blood cells like bone marrow and peripheral blood. These efforts have their own shortcomings such as the delay in sourcing the listed donor and the donor refusing to donate during need or because the listed donor has contracted an infection.
So how do we solve the current issue of finding matching stem cell units? Today what we need is an organised umbilical cord blood banking system in the country which could treat patients in need and be used for further medical research.
With the need for unrelated umbilical cord blood stem cells and the current day challenges in the Public cord blood banks, there is a huge need for a common pool of stem cell banks. This module would offer the entire family the access to their baby’s stem cells and also the common pool of stem cells from other members who can act as donors too.
It would be easy for a country like India to make a large inventory umbilical cord banking covering even rare ethnic groups due to the high birth rate amidst the Indian populace.
Seventy per cent of the patients of Indian origin who don’t find a matching bone marrow donor would benefit immensely through the sharing model. Through community banking of cord blood units, India has the potential to become the largest inventory of stem cells globally, increasing the scope of potentially lifesaving stem cell transplants for babies, their families, their communities and others of Indian origin worldwide.
With increasing trend of parents preserving their baby’s stem cells, community stem cell banking would help increase the inventory by more than 50,000 every year. By this, there is a >90 per cent chance for patients in India to find a match if the inventory exceeds 250,000 units.
In the recent past, to extend the treatment for fatal blood-related conditions to the tribals suffering with Sickle Cell Anaemia, the government has also passed a bill in parliament on the necessity of large inventory of unrelated stem cell banks.
(Mayur Abhaya Srisrimal is Chief Executive Officer & Managing Director, LifeCell. The views expressed are personal. He can be contacted at mayur.a@lifecell.in)
—IANS
by Editor | May 25, 2021 | Opinions
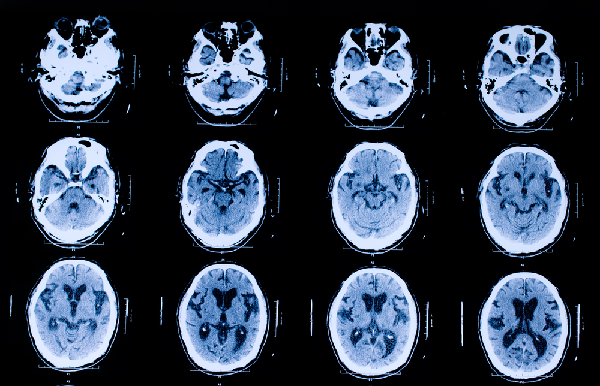
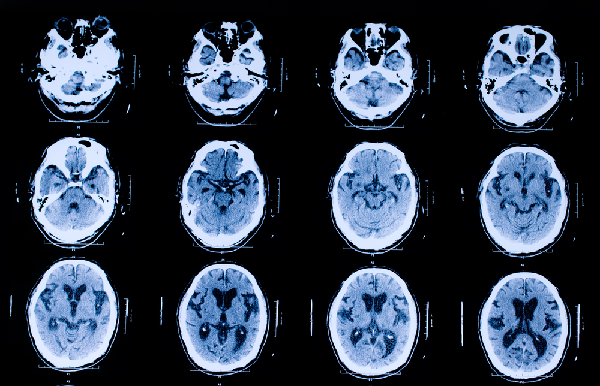
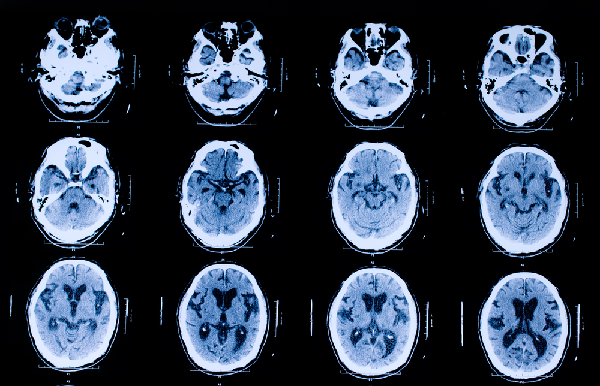 Huddersfield, England, (IINA) – Doctors are increasingly using computerized tomography (CT) scans in order to more accurately diagnose patients, but, concerns have been raised about the increased risk of cancer in people who have undergone these scans, Mail Online health news reported quoting Health risk Professor Bob Heyman from University of Huddersfield.
Huddersfield, England, (IINA) – Doctors are increasingly using computerized tomography (CT) scans in order to more accurately diagnose patients, but, concerns have been raised about the increased risk of cancer in people who have undergone these scans, Mail Online health news reported quoting Health risk Professor Bob Heyman from University of Huddersfield.
A CT scan (or ‘CAT scan’) provides doctors with a much clearer picture of what is happening inside the body than conventional X-rays. But these machines also deliver a much higher dose of ionizing radiation.This not only causes tissue damage, but can increase the risk of cancer.
The increase in risk is proportional to the amount of radiation received. Risk accumulates with repeated exposure, and children are more susceptible than adults.
Because CT scans require many images to be taken in the same body area, they deliver more radiation than a conventional X-ray.For example, 50 times more radiation in the abdominal area has been detected. But a 50-fold increase in a very small number is still a small number.
It has been estimated that an abdominal scan delivers about six times as much ionizing radiation as a person would receive from the environment in a year. Authors of a large UK study found that children exposed to higher radiation doses from CT scans faced threefold increases in their risks of developing leukaemia and brain tumours compared with those who received lower doses.
The higher the amount of radiation the children received, the greater their chances of developing these cancers were. The number of children diagnosed with either cancer over a 17-year period was about 200 out of 180,000 who were scanned.About 170 of these 200 children would, according to the researchers, have developed cancer as a result of having had higher radiation exposure from CT scans.
They were chosen because the authors considered them to be most affected by radiation exposure.The overall estimated risk was therefore 170 in 180,000, or about one in a thousand. But there are methodological problems with this and similar research.
Some 30,000 children could not be included in the data analysis, mainly because their medical records were incomplete, and their omission might have affected the findings. And, although the researchers attempted to do so, we cannot rule out ‘reverse causation’, that is, some children having had more CT scans because they had underlying health problems, rather than vice versa.
The researchers excluded children who were given CT scans because cancer was suspected. And as the authors acknowledge, this approach has limitations.
Children who receive CT scans may differ from those who do not in unknown ways which also make the former more likely to develop cancer.The only way to definitively exclude reverse causation would be to do a randomized controlled trial.
This would involve randomizing children into higher and lower exposure groups and following them up over a long period to see how many in each group developed cancer.This would, of course, be totally unethical.
Also, the findings don’t exclude the possibility that children who have CT scans become at greater risk of experiencing other diseases, or over longer time periods than were considered in the study.
Reverse causation might result in the risk from scans being overstated because the children who had more scans might have been more likely to develop cancers even if they had not been exposed to extra radiation.On the other hand, exclusion of other conditions and longer time periods might lead to the risk from scans being understated.
Overall, there is considerable uncertainty about the risk estimates generated by the study. Using UK data similar to that outlined above, researchers in the US concluded that about 2 per cent of US cancers would be caused by radiation from CT scans.
This conclusion is subject to the same cautions as detailed above. Also, the absence in the US of centralized databases of health records adds further complications to risk estimates.